Managing RRD in GDD eyes Sharma U et al evaluated the outcome of rhegmatogenous retinal detachment (RRD) surgery in eyes with preplaced glaucoma drainage device (GDD) with respect to intraocular pressure (IOP) control as well as success of retinal detachment (RD) surgery. In this retrospective case series, case records of patients who underwent RD surgery after GDD implantation from 2000 to 2014 were screened. The demographicdata, ocular examination findings at all visits, details pertaining to retinal detachment and its repair, and the postoperative course was documented. Twelve patients were included in the study. The mean age of patients was 24.3 years (median 11 years; range 3-72 years). Male: Female ratio was 3:1. Mean duration between GDD and RD was 24 months (4 days-91 months). Of the ten eyes that underwent surgery, nine eyes underwent pars plana vitrectomy, and in one eye scleral buckling was done. GDD was removed only in one eye. At final follow-up, retina was attached with controlled IOP in 6 (60%) eyes, of which 5 (50%) had improvement in best corrected visual acuity. The series showed that pars plana vitrectomy was required in almost all cases for the management of RD in eyes with preplaced GDD. Retinal reattachment with good IOP control could be achieved in 60% of eyes. Removal of the drainage device was not essential for the effective management of the RRD in most cases. With multidisciplinary approach, close follow-up and timely intervention, vision can be preserved along with glaucoma control and successful retinal reattachment.
Read More:
Sharma U et al. Outcomes of rhegmatogenous retinal detachment surgery in eyes with pre-existing glaucoma drainage devices. Indian J Ophthalmol. 2018 Dec;66(12):1820-1824
Does posterior vitreous detachment make intravitreal injections less effective?
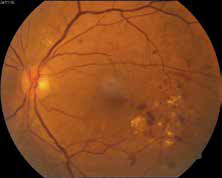
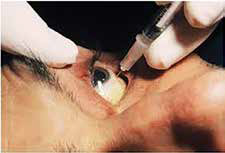
Neudorfer et al conducted a prospective cohort study investigating the effect of posterior vitreous detachment (PVD) on the efficacy of intravitreal bevacizumab for exudative age-related macular degeneration (AMD), in view of evidence that the vitreoretinal interface impacts the severity of the disease. Treatment-naïve AMD eyes with (+) complete PVD and without (-) PVD on ultrasonography received three monthly and then pro re nata bevacizumab injections. Bestcorrected visual acuity (BCVA) on Snellen charts and optical coherence tomography (OCT) findings were recorded for 12 months. Secondary analysis included PVD definition and group allocation according to OCT baseline scan. Forty-one eyes of 34 patients met the inclusion criteria. At 12 months, median BCVA improved by 0.12 logMAR in the PVD+ group [interquartile range (IQR) -0.52, 0.03, P = 0.140] and remained the same in the PVD- group (IQR -0.12, 0.15, P = 0.643). Median central retinal thickness improved by 43.5 μm and 43 μm in the PVD+ (IQR -143, 3, P = 0.016) and PVD- group (IQR -90, -14, P = 0.008), respectively. All parameters were similar in the two groups at final follow up (P > 0.05). The secondary analysis included 32 eyes of 26 patients and showed no significant differences between the groups at the 12 months endpoint (P > 0.05). The study concluded that there was no significant impact of PVD as assessed by ultrasound or by OCT on visual and anatomical outcomes in exudative AMD treated with bevacizumab.
Read More:
Neudorfer M et al. The role of posterior vitreous detachment on the efficacy of anti-vascular endothelial growth factor intravitreal injection for treatment of neovascular age-related macular degeneration. Indian J Ophthalmol. 2018 Dec;66(12):1802-1807.