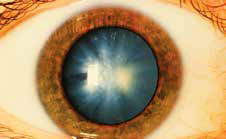
Cataract surgery in eyes with optic neuropathy: To do or not to do?
Aggarwal et al compared the visual acuity outcomes of cataract surgery between patients with and without non-glaucomatous optic neuropathies. They undertook a retrospective case-control study of patients with and without optic neuropathies who underwent cataract surgery from 2010 to 2017. For all eyes, the last preoperative best corrected visual acuity (BCVA) and first BCVA greater than 1 month postoperatively (to ensure sustained refractive stabilization) were recorded in logarithm of the minimum angle of resolution (logMAR) units. Thirty patients (42 eyes) with optic neuropathies and 30 control patients (42 eyes) underwent uncomplicated cataract surgery. The mean age at surgery was significantly younger in the optic neuropathy group (64 versus 71.2 years, p < 0.01). The mean improvement in visual acuity in the optic neuropathy group was 0.4 ± 0.6 logMAR units (roughly 4 Snellen lines) from 0.7 ± 0.8 units preoperatively to 0.3 ± 0.5 postoperatively. Between the cases and controls, there was no significant difference in preoperative BCVA(p = 0.48), postoperative BCVA (p = 0.42), or the mean improvement in BCVA (p = 0.82). When stratified by optic neuropathy subtype, patients with optic neuropathies secondary to multiple sclerosis (n = 12) or non arteritic ischaemic optic neuropathy (n = 11) had significant improvement in BCVA postoperatively (p < 0.01 and p = 0.03, respectively). The authors concluded that contrary to what may be expected from such a severe ocular comorbidity, data suggest that the mean BCVA improvement after cataract surgery in patients with nonglaucomatous optic neuropathies was comparable to that of control patients. Cataract surgery may be performed in patients with both optic neuropathies and advanced cataracts with a reasonable preoperative expectation that visual acuity improvement can be significant.
Read More:
Aggarwal S et al. Visual acuity after cataract surgery in patients with optic neuropathies. Acta Ophthalmol. 2018 Dec 3.
What makes an anterior capsulorhexis strong?
Daya et al and other researchers from the Singapore National Eye Centre, Singapore, and CapsuLaser Inc., Livermore, California, USA studied the effects of anterior capsulotomy diameter and discontinuity on tear threshold load and distension for the technique of continuous curvilinear capsulorhexis (CCC). They performed two separate randomized pairwise cadaver eye preclinical studies. Capsulotomies were performed in 40 cadaver eyes of 20 donors using CCC. The pairwise comparisons were divided into 2 study groups: Study A: Continuous versus discontinuous capsulotomies; Study B: Capsulotomy diameter of 5.0 mm and smaller versus diameters of 5.2 mm and larger. A shoe-tree method was used to apply load to the capsulotomy rim, and the Instron tensile stress instrument measured threshold load and distension to initiate a capsular tear. Wilcoxon matched-pairs signedrank tests were performed to assess statistical superiority. The results showed that in study group A, all pairs demonstrated that continuous capsulotomies were better than discontinuous capsulotomies for both the anterior tear threshold load and distension (P < .01). In study group B, 80% of the pairs demonstrated that diameters of 5.2 mm and larger were better than those of 5.0 mm and smaller diameter (P < .05). The study concluded that anterior capsulotomies behave as nonlinear elastic (elastomeric) systems when exposed to an external load and distension. This study demonstrated that continuous circular capsulotomies were more resistant to anterior tears than discontinuous capsulotomies. A point of irregularity or a defect in a capsulotomy rim has a high probability of being the tear initiation point. Furthermore, larger diameter capsulotomies were more resistant to anterior tears than smaller capsulotomies.
Read More:
Daya SM et al. Parameters affecting anterior capsulotomy tear strength and distension. J Cataract Refract Surg. 2018 Nov 30.