
Dr Chaitra Jayadev
Narayana Nethralaya Eye Institute
Bangalore
Dr Arpitha Pereira
Narayana Nethralaya Eye Institute
Bangalore
It is said that things move fast in the world of modern medicine. The field of medical retina appears to be no exception, with numerous developments taking place, such as introduction of new drugs, new treatment modalities and imaging techniques. While a detailed description is out of the scope of this article, we hope to give you a glimpse into what is new in the world of medical retina.
Newer Imaging Modalities: We describe a few imaging modalities that have become popular recently.
1. Wide-field Imaging:
Conventional fundus imaging typically generates images with a 30 to 50-degree field of view, corresponding to approximately 5% to 15% of the retinal surface area. This allows for visualization of the posterior pole but not the Dr Chaitra Jayadev narayana nethralaya eye institute, bangalore retinal periphery. The Optos system (Optos, Dunfermline, Scotland), through the use of a large ellipsoid mirror with 2 focal lengths (allowing wide scanning angles) and an SLO, provides image capture with a 200 degrees internal field of view (approximately equivalent to 135 to 150 degrees external field of view). The system provides the ability to capture red and green reflectance imaging, as well as fundus autofluorescence, and fluorescein/indocyanine green angiography (1). Ultra-Widefield Angiography (UWFA) has been shown to demonstrate abnormalities in a variety of retinal conditions, including diabetic retinopathy, retinal vein occlusion, sickle cell retinopathy, uveitis, and pediatric retinal disease (2,3).
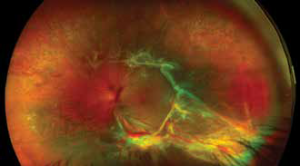
Figure 1: Wide-field Optos image of the left eye of a 55 year old diabetic female patient showing dense fibrovascular proliferation involvin the posterior pole and its peripheral extension
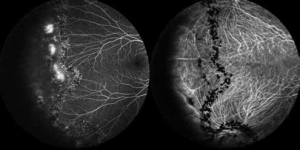
Figure 2: Wide field combined fundus fluorescein and indocyanine green angiography in a 30-year-old male patient demonstrating peripheral vascular leak
2. MultiColor Imaging:
MultiColor scanning laser imaging is a new technology for fundus imaging offering detail and clarity not available from traditional fundus photography. MultiColor images are captured by simultaneously scanning with three individual laser wavelengths: blue, green, and infrared. The different wavelengths penetrate the tissue to different depths and therefore provide structural information from different depths within the retina (4).
3. Wide Field OCT
(Fremont, CA) Avanti RTVue- XR widefield system uses SD technology and can obtain 70,000 A-scans/second. The Avanti RTVue-XR can create 12 mm x 9 mm B-scans, and its active eye tracking enhances image stability. Wide field OCT can provide detailed information of the lesions that are present away from the arcade. These are very useful imaging modalities for conditions like choroidal tumors and peripheral lesions such as retinoschisis (5–7).
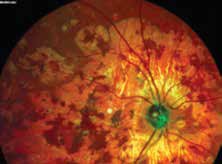
Figure 3: Multicolour OCT image of the right eye of a
50-year-old female patient showing healed choroidal
patches of serpigineous choroiditis
4. Hand Held OCT: Spectraldomain OCT systems (Bioptigen Envisu SDOIS; Bioptigen, Research Triangle Park, NC, USA) with handheld imaging probes connected to a table-top console by a 1.3-m-long cable is a device which has now been used widely in imaging pediatric disorders. It has been proven particularly useful in neonatal populations for the study of ocular development and for diseases such as retinopathy of prematurity
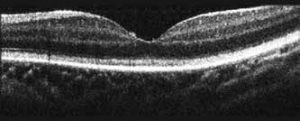
Figure 4: A spectral domain-optical coherence tomography image
using the Envisu 2300 (Bioptigen Inc., Research Triangle Park, NC, USA)
of a 1-year old female child with a cone-rod dystrophy demonstrating an
absent foveal tent and an irregularly thickened and hyperreflective
layer of cone outer segment tips
5. Adaptive optics: Optical retinal imaging modalities rely on the optical elements of the eye itself (mainly the cornea and lens) to produce retinal images. As a results of imperfections in these structures, aberrations are introduced to the imaging light and image quality is degraded. To compensate for these aberrations, adaptive optics (AO) along with optical coherence tomography (OCT) have been utilized (9). This enabled for the first time in vivo volumetric retinal imaging with high isotropic resolution. Using adaptive optics, photoreceptor loss/changes can be imaged.
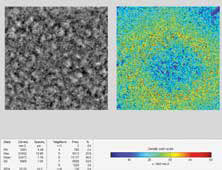
Figure 5: Adaptive optics imaging
of the left eye fovea of a healthy 25-year-old
male showing normal average cone count
and distribution
6. Optical coherence tomography angiography (OCTA): OCTA is a new non-invasive imaging technique that employs motion contrast imaging to highresolution volumetric blood flow information generating angiographic images in a matter of seconds. OCTA compares the decorrelation signal (differences in the backscattered OCT signal intensity or amplitude) between sequential OCT b-scans taken at precisely the same cross-section in order to construct a map of blood flow .The two main types of OCTA instruments are spectral-domain OCTA (SDOCTA) and swept-source OCTA (SS-OCTA). Both use Fourier domain detection techniques, but the SD-OCT instruments use a broadband near-infrared super luminescent diode as a light source, currently with a center wavelength of approximately 840 nm, with a spectrometer as the detector, while SS-OCT devices use a tunable swept laser while SS-OCT devices use a tunable swept laser, currently with a center wavelength of approximately 1,050 nm, with a single photodiode detector. The main advantage of SS-OCTA imaging over SD-OCTA is a faster scanning speed, which allows for denser scan patterns and larger scan areas than SD-OCTA scans for a given acquisition time. Another advantage of the current SS-OCTA technology is that it uses a longer center wavelength that can reduce sensitivity rolloff of the signal under the RPE, which results in enhanced light penetration into the choroid and better detection of signals from the deeper layers.

Figure 6a: Fundus fluorescein Angiography of the left eye of a 68-year-old diabetic man,
demonstrating intense hyperfluourscence adjacent the infero-temporal arcade suggestive of
neovascular complex. The outline of the new vessel is obscured by the leakage of the dye.
New treatment options:
Age Related Macular Degeneration (AMD): While tremendous progress has been made in the field of wed AMD, there still appears to be no treatment for dry AMD. Here we take a look at some treatment options which may become viable in the near future.
1. Photobiomodulation involves application of visible to nearinfrared light to cells to produce beneficial effects. A recent study on 42 patient with dry AMD showed that application of multiwavelength light composed of yellow (590 nm), red (670 nm) and near-infrared (790 nm) for a period of 3 weeks resulted in significant improvement in BCVA, contrast sensitivity, and the drusen size.
2. Brimonidine is a selective alpha-2 receptor adrenergic agonist with additional neuroprotective properties (15). Phase II clinical trial to evaluate the safety and efficacy of a brimonidine tartrate intravitreal implant (Brimo DDS, Allergan) in patients with dry AMD showed that Brimo DDS reduced the rate of progression at 1 year
3. Minocycline is a tetracycline derivative with neuroprotective properties. Presently, there are ongoing phase II trials that are evaluating the effects of oral minocycline (100 mg, twice daily) and doxycycline (40 mg, daily) in the treatment of AMD patients with geographic atrophy.
4. Lampalizumab is a humanized IgG Fab fragment that inhibits complement factor D and showed promise in initial studies. However, the 2 phase III trials Chroma and Spectri showed tha lampalizumab failed to impact the geographic area compared to sham treatment.
Diabetic Macular Edema: While there is no doubt that anti–VEGF-A monotherapy has revolutionized the treatment of diabetic macular edema (DME), there still remains a subset of patients who are non-responders. The unmet need presented by these patient forms the impetus for developing new options for the treatment of DME. We enumerate a few that show promise
1. Next-generation anti–VEGF-A drugs
a. Conbercept is a recombinant human VEGF receptor-Fc fusion protein, which inhibits VEGF-A, VEGF-B, and placental growth factor (PlGF). The FRONTIER and SAILING studies showed improvement in visual acuity and concomitant decreases in retinal thickness on OCT in patients with DME
b. Abicipar Pegol belongs to the class of genetically engineered antibody mimetic proteins called designed ankyrin repeat proteins (DARPins). Results from the phase 2 PALM study showed that abicipar pegol, injected every 8 or 12 weeks in patients with DME, offered functional and anatomic effects similar to those of ranibizumab injected monthly.
2. Angiopoietin combination drugs: Angiopoietin plays an important role in angiogenesis. In health, angiopoietin-1 (Ang-1) is crucial for vessel development. In disease states, Ang-2 is upregulated. This cytokine is an antagonist of Ang- 1, which attracts proangiogenic and inflammatory cytokines. Its activation is often coupled with upregulation of VEGF-A, causing increased vascular permeability. Two products in this category RG7716 (Genentech/Roche) and a combination of the Ang- 2 antibody nesvascumab plus aflibercept are currently being studied.
Other combination drugs in the pipeline include OPT 302 (“trap” molecule binds and neutralizes the activity of VEGF-C and VEGF-D by), ALG-1001 (intergrin peptide therapy) and KVD001 (protease inhibitor that targets plasma kallikrein).
3. Suprachoroidal corticosteroid: The injection of triamcinolone acetonide (CLS-TA; Clearside Biomedical) into the suprachoroidal space is a novel approach to the treatment of patients with DME. The HULK clinical trial examined suprachoroidal CLS-TA with and without intravitreal aflibercept and showed signs of increased efficacy and durability with the investigational drug.
References
1. Witmer MT, Parlitsis G, Patel S, Kiss S. Comparison of ultrawidefield fluorescein angiography with the Heidelberg Spectralis® noncontact ultra-widefield module versus the Optos® Optomap®. Clin Ophthalmol. 2013;7:389–94.
2. Patel RD, Messner L V, Teitelbaum B, Michel KA, Hariprasad SM. Characterization of ischemic index using ultrawidefield fluorescein angiography in patients with focal and diffuse recalcitrant diabetic macular edema. Am J Ophthalmol. 2013;155(6).
3. Dai S, Chow K, Vincent A. Efficacy of wide-field digital retinal imaging for retinopathy of prematurity screening. Clin Exp Ophthalmol. 2011;39(1):23–9.
4. Tan ACS, Fleckenstein M, Schmitz-Valckenberg S, Holz FG. Clinical Application of Multicolor Imaging Technology. Ophthalmologica. Karger Publishers; 2016;236(1):8–18.
5. Povazzay B, Hermann B, Hofer B, Kaji V, Simpson E, Bridgford T, et al. Wide-field optical coherence tomography of the choroid in vivo. Investig Ophthalmol Vis Sci. 2009;50(4):1856–63.
6. Mori K, Kanno J, Gehlbach PL. Retinochoroidal morphology described by wide-field montage imaging of spectral domain optical coherence tomography. Retina. 2016;36(2):375–84.
7. McNabb RP, Grewal DS, Mehta R, Schuman SG, Izatt JA, Mahmoud TH, et al. Wide field of view swept-source optical coherence tomography for peripheral retinal disease. British Journal of Ophthalmology. 2016;
8. Vinekar A, Mangalesh S, Jayadev C, Maldonado RS, Bauer N, Toth CA. Retinal Imaging of Infants on Spectral Domain Optical Coherence Tomography. Biomed Res Int. Hindawi; 2015 Jul 6;2015:782420.
9. Pircher M, Zawadzki RJ. Review of adaptive optics OCT (AO-OCT): principles and applications for retinal imaging [Invited]. Biomed Opt Express. Optical Society of America; 2017 May 1;8(5):2536.
10. Song H, Rossi EA, Latchney L, Bessette A, Stone E, Hunter JJ, et al. Cone and rod loss in stargardt disease revealed by adaptive optics scanning light ophthalmoscopy. JAMA Ophthalmol. 2015;133(10):1198–203.
11. Jacob J, Krivosic V, Paques M, Tadayoni R, Gaudric A. Cone density loss on adaptive optics in early macular telangiectasia type 2. Retina. 2016;36(3):545–51.
12. Choi WJ, Mohler KJ, Potsaid B, Lu CD, Liu JJ, Jayaraman V, et al. Choriocapillaris and choroidal microvasculature imaging with ultrahigh speed OCT angiography. PLoS One. 2013;8(12).
13. de Carlo TE, Romano A, Waheed NK, Duker JS. A review of optical coherence tomography angiography (OCTA). Int J Retin Vitr. BioMed Central; 2015 Apr 15;1(1):5.
14. Merry GF, Munk MR, Dotson RS, Walker MG, Devenyi RG. Photobiomodulation reduces drusen volume and improves visual acuity and contrast sensitivity in dry age-related macular degeneration. Acta Ophthalmol. 2017;95(4):e270–7.
15. Doozandeh A, Yazdani S. Neuroprotection in glaucoma. Journal of Ophthalmic and Vision Research. 2016. p. 209–20.
16. Kuppermann BD et al. Brimonidine drug delivery system generation 1 in patients with geographic atrophy: Post
hoc analysis of a phase 2 study [Internet]. [cited 2018 Apr 5]. Available from: https://www.healio.com/ophthalmology/retina-vitreous/news/online/%7B7e23cf82-d686-4125-ac42-0f6c610dc44b%7D/intravitreal-implant-withbrimonidine-reduced-ga-lesiongrowth-in-phase-2-study.
17. Evaluation of Oral Minocycline in the Treatment of Geographic Atrophy Associated With Age- Related Macular Degeneration – Full Text View – ClinicalTrials. gov [Internet]. [cited 2018 Apr 5]. Available from: https://clinicaltrials.gov/ct2/show/NCT02564978
18. Yates Paul. Clinical Study to Evaluate Treatment With ORACEA® for Geographic Atrophy (TOGA) – Full Text View – ClinicalTrials.gov [Internet]. [cited 2018 Apr 5]. Available from: https://clinicaltrials.gov/ct2/show/NCT01782989
19. Safety and efficacy by multiple injection of KH902 in patients with diabetic macular edema (DME) (Frontier-1). https://clinicaltrials.gov/ct2/show/NCT01324869.
20. Safety and efficacy study of conbercept in diabetic macular edema (DME) (Sailing). https://clinicaltrials.gov/ct2/show/NCT02194634.
21. Hassan TS. A multicenter, double masked phase 2 clinical trial evaluating abicipar pegol for diabetic macular edema. Paper presented at: American Academy of Ophthalmology Annual Meeting; October 14-18, 2016; Chicago.
22. Wykoff CC. Suprachoroidal triamcinolone acetonide with and without intravitreal aflibercept for diabetic macular edema: Phase 1/2 HULK study. Paper presented at American Academy of Ophthalmology Retina Subspecialty Day; November 10- 11, 2017; New Orleans.
