Is your patient complying to face down positioning?
Prone or face-down positioning of patients after a macular hole surgery is considered critical to the success of hole closure. However, it is common to see patients not complying to the position due to the discomfort involved. A paper published recently aimed to determine adherence to face-down positioning (FDP) among patients 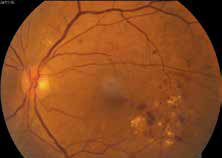 who underwent vitrectomy and gas tamponade for macular hole (MH) repair. A total of 69 patients (37 females and 32 males) were studied and nurses recorded whether the patient complied with the position each time they examined the patient. A FDP score was obtained from the nursing records; patients were given a score of 1 if they complied with the FDP and 0 if they did not. The score was recorded four times per day for the first 3 postoperative days. A perfect FDP score was 12. The mean ± standard deviation of the FDP scores was 10.6±1.8 (range: 4-12). Less than half (46.4%) patients scored a perfect 12, and 10% patients scored <8. Failure of the MH closure was observed in only one patient (1.4%), who showed the poorest adherence to FDP (score =4). Also, the closure rate in patients with FDP score <7 (2/3, 66.7%) was significantly lower than in patients with an FDP score ≥7 (66/66, 100%) (P<0.05, Fisher’s exact probability test). The authors had also published a previous study of FDP compliance in vitrectomy for rhegmatogenous retinal detachments and found an even worse compliance. They concluded that the poor adherence to FDP can negatively impact the effectiveness of the surgery for MH repair.
who underwent vitrectomy and gas tamponade for macular hole (MH) repair. A total of 69 patients (37 females and 32 males) were studied and nurses recorded whether the patient complied with the position each time they examined the patient. A FDP score was obtained from the nursing records; patients were given a score of 1 if they complied with the FDP and 0 if they did not. The score was recorded four times per day for the first 3 postoperative days. A perfect FDP score was 12. The mean ± standard deviation of the FDP scores was 10.6±1.8 (range: 4-12). Less than half (46.4%) patients scored a perfect 12, and 10% patients scored <8. Failure of the MH closure was observed in only one patient (1.4%), who showed the poorest adherence to FDP (score =4). Also, the closure rate in patients with FDP score <7 (2/3, 66.7%) was significantly lower than in patients with an FDP score ≥7 (66/66, 100%) (P<0.05, Fisher’s exact probability test). The authors had also published a previous study of FDP compliance in vitrectomy for rhegmatogenous retinal detachments and found an even worse compliance. They concluded that the poor adherence to FDP can negatively impact the effectiveness of the surgery for MH repair.
Read More:
Shimada Y, Seno Y, Mizuguchi T, Tanikawa A, Horiguchi M. Patient adherence to the face-down positioning after macular hole surgery. Clin Ophthalmol. 2017 Jun 8.
Macular hole after RRD repair
Full thickness macular holes have been not infrequently seen after rhematogenous retinal detachment (RRD) repair. A retrospective interventional case series was recently published in Retina where 25 patients who developed full thickness macular holes after successful RRD repair were included. RRD repair was done by pneumatic retinopexy (24%), scleral buckle alone (20%), pars plana vitrectomy only (32%), and combined scleral buckle and pars plana vitrectomy (24%). In 3/4th cases, the preceding RRD involved the macula before the formation of the macular hole. The median time to full-thickness macular hole diagnosis after RRD repair was 63 days. An epiretinal membrane was present in all 25 (100%) macular holes. Two macular holes (8%) spontaneously closed, whereas the other 23 (92%) were successfully closed after a single surgical procedure. The study demo started that full-thickness macular hole formation can occur after all types of RRD repair and is associated with an epiretinal membrane. The epiretinal membrane may play a role in the pathogenesis of secondary macular hole formation after RRD repair.
Read More:
Khurana RN, Wykoff CC, Bansal AS, Akiyama K, Palmer JD, Chen E, Chang LK, Major JC Jr, Wu C, Wang R, Croft DE, Wong TP. The Association of Epiretinal Membrane with macular hole formation after rhegmatogenous retinal detachment repair. Retina. 2017 Jun;37(6): 1073-1078.
Update on the Epidemiology of Age-Related Macular Degeneration
This study is a meta-analysis reports on current estimates of the prevalence of age-related macular degeneration (AMD) based on a review of recent meta-analyses and literature research. Within an age of 45-85 years, global prevalences of any AMD, early AMD, and late AMD were 8.7%, 8.0% and 0.4% . Early AMD was more common in individuals of European ancestry than in Asians, whereas prevalence of late AMD did not differ significantly. AMD of any type was less common in individuals of African ancestry. The number of individuals with AMD was estimated to be 196 million (95% CrI, 140 – 261) in 2020. The worldwide number of persons blind or with moderate to severe vision impairment due to macular disease in 2010 was 2.1 million and 6.0 million respectively. (95% UI, 5.2 – 8.1) persons out of 191 million people with MSVI. Agestandardized prevalence of macular diseases as cause of blindness in adults aged 50+ years worldwide decreased from 0.2% in 1990 to 0.1% in 2010; as cause for visual impairement, it remained mostly unchanged at 0.4% in 1990 to 0.4% in 2010. These data show the globally increasing importance of AMD.
Read More:
Jonas JB, Cheung CMG, Panda-Jonas S. Updates on the Epidemiology of Age- Related Macular Degeneration. Asia Pac J Ophthalmol (Phila). 2017 Sep 14.
Portable non-mydriatic versus standard fundus cameras?
In the recent few years a number of portable non mydriatic fundus cameras have hit the market. They carry an advantage of size and are projected as ideal tools for screening camps. Are they as good as the standard fundus cameras? This study evaluated the sensitivity and specificity of a portable non-mydriatic fundus camera to diagnose visionthreatening diabetic retinopathy (VTDR). A prospective, single-site, comparative instrument validation study was undertaken at the Aravind Eye Care System where 155 subjects with and without diabetes were examined with
(1) non-mydriatic Smartscope,
(2) mydriatic Smartscope, and
(3) mydriatic table-top camera of the
macular, nasal, and superotemporal fields. A retina specialist performed a dilated fundus examination and was the reference standard. Two masked retina specialists graded the images. Sensitivity and specificity to detect VTDR with the undilated Smartscope was calculated compared to dilated clinical fundus exam. The study found that remote graders had high sensitivity and specificity in diagnosing VTDR with undilated Smartscope images, suggesting utility
where portability is a necessity. It was comparable to that of a table top standard fundus camera.
Read More:
Sengupta S, Sindal MD, Besirli CG, Upadhyaya S, Venkatesh R, Niziol LM, Robin AL, Woodward MA, Newman Casey PA. Screening for visionthreatening diabetic retinopathy in South India: comparing portable non-mydriatic and standard fundus cameras and clinical exam. Eye (Lond). 2017 Sep 15.