Dr. Digvijay Singh, MD, Faico
Director, Noble Eye Care
Gurugram
Technological progress in ophthalmology has led surgical progress. Since the advent of cataract, glaucoma or retinal surgery, ophthalmologists and biomedical engineers have strived to enhance the precision and safety of surgery by providing technological solutions to biological problems. These include replacement of manual procedures with machines and enhancing the ease of various surgical steps. This article describes some of the latest technological advances and devices used for ophthalmic surgery including a few which are just around the horizon
New devices in cataract surgery
Cataract surgery has come a long way since the advent of the intraocular lens and operating microscope. Extracapsular cataract surgery created the requirement for a capsulotomy and phacoemulsification furthered that to a curvilinear continuous capsulorrhexis. A lot of the latest technology and devices in cataract surgery are focussed on improving this one important step of cataract surgery: capsulorrhexis. These include the Femtosecond laser, Zepto and CAPSUlaser among others. Some of these and other new devices in cataract surgery are described below and in other articles in this issue.
1. Zepto
The Zepto capsulotomy system (Mynosys Cellular Devices, Fremont, California) is a device for making a capsulotomy. It consists of a thin nitinol wire loop, which is the element that gets hot and does the cutting. The loop is surrounded by a silicone plastic shell connected to a suction tube. The silicon shell can be introduced into the eye through a 2.2 mm incision and a wire loop can be extended through the silicon shell onto the capsule. The size of the loop is modified by the amount of push or pull applied to the nitinol wire through a push rod. Once the nitinol circular ring is placed on the capsule, a suction is turned on which makes the loop stick to the capsule and then a jolt of electricity is passed through it which cuts the capsulotomy. The suction is then released and the loop is pulled back. The silicon shell is then withdrawn out through the corneal wound. The disposable handpiece under the ring is all one unit with a cord that plugs into a box. The zepto box is a one-time purchase and is used for many patients. The main concern with this technology is the cost, however overall, the cost is much lesser than the Femtosecond laser
The Zepto capsulotomy system in action
2. ApertureCTC
ApertureCTC (International BioMedical Devices, Mt. Pleasant, South Carolina) is somewhat similar to the Zepto. It is a device which uses thermal energy to create a capsulotomy. The tip design is stainless steel and does not require suction, both of which are different from the Zepto. It has two compressible stainless steel blades that form a perfect circle. When they are in the elongated position, they can be introduced through a 2.2-mm incision. A slider on the handpiece, compresses the blades to form a circle and then a current is run through the blades, which creates heat, and cuts the capsule tissue in milliseconds. Since there is no suction and silicon sleeve, the thermal heating element has to be insulated from the anterior chamber environment by the use of viscoelastic. It should be available for human use in a couple of years.
ApertureCTC handpiece and tip
3. CAPSULaser
CAPSULaser (Los Gatos, California) is a laser device that attaches to the operating microscope and can make capsular openings from 4.5 mm to 6.5 mm. The capsular opening is created in 1 second following staining of the anterior capsule with a new formulation of trypan blue. It is slated to be better than the femtosecond laser in terms of accuracy of sizing, circularity, and centration on the visual axis.
CAPSULaser system attached to the operating microscope
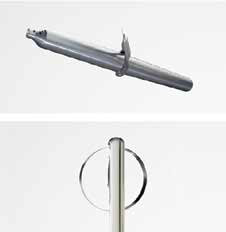
4. miLoop miLoop
(Iantech, Reno, Nevada) is an endocapsular, nitinol ring that acts like a snare and bisects the cataract and chops the cataract into smaller pieces. It is expected to be an alternative or supplement to the femtosecond laser and can be used in complex and dense hard cataracts. Its unique advantages is that it truly bisects the cataract from equator to equator, even behind a small pupil, unlike any other technology including the femtosecond laser which only breaks what it can see and causes an incomplete chop. The miLoop can chop the cataract into smaller pieces if deployed multiple times. When is use, it would make the surgery easier by dismantling the lens and mobilizing the fragmented pieces making them easier to aspirate. It would also decreases ultrasound energy levels inside the eye in denser cataracts, which allows for faster healing and fewer complications. However, there is a disposable cost to this, though it would be much cheaper than the femtosecond laser. The good thing about the miLoop is that it can be used through a scleral tunnel and therefore be useful in SICS surgery too.
miLoop Handpiece
All these devices eliminate the capsulorrhexis and nuclear chopping which are the most difficult parts of cataract surgery, so the learning curve is not steep. While these would be very helpful for surgeons under training, they may seem a bother to those who are well versed in these skills and actually seem to increase costs. However, considering lower rates of complications, early wound healing and a better refractive outcome, they will prove to be useful tools for all.
New devices for glaucoma surgery
Glaucoma surgery has always been unpredictable with a lower safety profile than cataract surgery and even though there has been immense progress such as the use of antifibrotics and drainage implants, a perfect surgical solution seems far.
Stent technology is a familiar modality in cardiovascular, pulmonary, gastrointestinal and other specialties. Of late, there have been multiple attempts to use this in ophthalmology and particularly glaucoma. Since a stent can not only bypass existing obstructions, but also introduce a new outflow pathway in a relatively minimally invasive surgery. A few new devices and modalities for glaucoma surgery are discussed below.
1. iStent
The original iStent (Glaukos, California) saw success in mild to moderate open angle glaucoma and was among the first such device to be commercially available. It was a tiny tubular device which was amongst the smallest used for glaucoma surgery. Now the next generation, iStent Inject is available. It is about one-third the size of the original iStent and is a solo device. The next gen iStent is often used in combination with cataract surgery and has resulted in dramatic reductions in IOP.
iStent
2. Hydrus Microstent
The Hydrus Microstent (Ivantis, California) is the first “intracanalicular scaffold” for primary open-angle glaucoma. The 7-mm stent is inserted into Schlemm’s canal to increase outflow by dilating and stabilizing the canal structure. It has been seen that upto a 40% reduction in IOP occurs with its use. It combines the advantages of conjunctiva sparring ab interno trabecular bypass with canal scaffolding and dilation.
Hydrus microstent
3. STARflo
The STARflo (iSTAR Medical, San Antonio) aims to augment the natural uveoscleral outflow. It is a silicone device with 27-μm pores which is inserted into the anterior chamber. The head of the device extends into the anterior chamber with the body curving through the sclera to the suprachoroidal space. IOP reduction of upto 60% has been documented at 12 months post insertion. It is a blebless device and requires ab externo surgery. An ab interno injectable MINIJect is also under development with a similar mechanism. The inert nature of the silicon used does not need use of antifibrotic agents.
StarFlo
4. CyPass Micro-Stent
The CyPass Microstent (Transcend Medical, California) is similar to the STARflo in that it drains directly into the suprachoroidal space, which offers a large absorptive capacity and a natural pressure gradient to drive outflow. However, it is slightly less efficacious with a reported IOP lowering of 35% at 2 years when combined with phacoemulsification. The next generation is the CyFlo Vx Infusion System, an injectable system that creates a reservoir to increase absorptive capacity. An additional 30- 40% drop over the CyPAss has been reported.
CyPass Micro-stent
5. Aquesys Xen
Aquesys Xen (Allergan, Dublin) is a gel stent, which bypasses the trabecular meshwork to create its own outflow into the subconjunctival space. The 6-mm stent with a 45 microns internal diameter uses flow mechanics to prevent hypotony. It creates an internal bleb which becomes a low-lying drainage area with fewer post-op complications and management issues than ab externo dissected blebs. An IOP reduction of 40% has been reported with its use. It may be used solo or combined with phacoemulsification.
Aquesys Gel Stent
6. Micro Shunt
Micro shunt (InnFocus, Florida) formerly known as MIDI Arrow has shown a dramatic drop in IOP (over 50%) from 23 mm Hg preinsertion to 10.9 mm Hg at 3 years in multinational studies. It is a drainage implant consisting of an extremely small micro-tube (about twice the size of an eyelash) that shunts aqueous fluid from the anterior chamber of the eye to a sub-conjunctival/sub-Tenon flap. The shunt is designed to be thin and soft to conform to the curvature of the eye. The device is made of SIBS, the most biostable thermoplastic elastomeric material currently in
existence.
InnFocus microshunt
7. Kahook Dual Blade (KDB)
New World Medical (New World Medical, Inc., California) is using research and marketing expertise gained with its Ahmed Glaucoma Valve to develop a novel device to improve outflow by removing a precise strip from the trabecular meshwork. The Kahook Dual Blade (KDB), uses twin blades to free juxtacanalicular trabecular meshwork and opens outflow with minimal collateral damage. This single-use, ophthalmic blade makes parallel incisions in the trabecular meshwork and inner wall of the Canal of Schlemm. The device has a microengineered profile which allows for insertion into the eye through a clear cornea micro incision. There is a stainless steel body comprised of a long, thin shaft that allows for access across the anterior chamber, a pointed tip used to pierce trabecular meshwork under gonioscopic view, a ramp that lifts and stretches the tissue as the device is advanced, and two blades which produce simultaneous incisions in the treated tissues. It may be used with or without cataract surgery to enhance natural drainage.
Kahook Dual Blade Device
8. TUG
Eye Sonix, California has recently developed a high frequency ultrasound called TUG which is aimed to be a first line therapy in naïve eyes or an adjunct in combination with medication. The current prototype unit delivers ultrasonic energy to a 1-mm treatment zone that encompasses the trabecular meshwork, open angle, and Schlemm’s canal at 12 locations around the eye. Ultrasound induces hyperthermia and sonomechanical vibrations that loosen blockages in the trabecular meshwork and trigger cytokine cascades to help reduce IOP.
Therapeutic ultrasound for glaucoma
(TUG)
9. EyeOP1
EyeOP1, a device similar to the EyeSonix one has been made by EyeTechCare, Lyon. It delivers ultrasonic energy using a suction cone coupled to the cornea. Energy is delivered to six 1-mm treatment areas around the eye. Ultrasonic energy removes the epithelial layers while preserving the underlying stroma. A nearly 30% reduction in IOP at 1 year with minimal side effects. The eyes remain quiet and no major side effects have been reported.
EyeOP1 in use
1. Vitrectomy systems
Eva vitrectomy system: The Eva (DORC, international) is a phacovitrectomy system with high speed (up to 16 000 cpm) two-dimensional cutting and a double cut and double aspiration cycle. Its VacuFlow fluid control system uses a feature called valve timing intelligence to eliminate unwanted pulsation and flow. It offers an efficient 92% duty cycle, creating a constant aspiration flow, independent of the cut speed, ideally reducing turbulence and traction on surrounding tissues. Additionally. the Eva’s LED endoillumination system offers a consistent quality of light and increased safety, with integrated ultraviolet and infrared filters. The system is available with 23-, 25-, and 27-gauge vitrectomy packs.
VersaVIT 2.0: The VersaVIT 2.0 vitrectomy machine (Synergetics, Baush and Lomb, New Jersey, US) features a cut rate of 6000 cpm and duty cycle control options. It is slated to be a portable system and includes a dual LED lighting.
Constellation: The Cosntellation CR4 Software upgrade (Alcon, Novartis, Fort Worth, Texas) is another recent product to enter the market. The software has a number of phaco and vitreoretinal enhancements. It supports a 10,000 cpm vitrector probe (Advanced Ultravit Vitrectomy Probe), the Autosert IOL injector, Ozil IP functionality for cataract surgery among other enhancements.
Stellaris PC Vision (Baush and Lomb, New Jersey, US) now features an adjustable chandelier fiber optic illuminator which delivers uniform, diffuse lighting and offers modifiable light control to provide better intraocular visibility and efficiency during vitreoretinal procedures. The chandelier works transsclerally or integrates seamlessly with the company’s Entry Site Alignment valved cannulas.
Eva Vitrectomy system
2. Handheld tools
23-Gauge Fragmentation Needle is available for the Stellaris PC Vision Enhancement System (Bausch + Lomb, New Jersey). The ultrasonic needle design can be used during vitreoretinal procedures to remove lens material from the posterior chamber. The idea is to eliminate the need to enlarge the sclerotomy, as was necessary when using the previous 20-gauge instrument.
Retractable Diamond Dusted Membrane Scraper is meant for use in internal limiting membrane (ILM) and epiretinal membrane removal, is now available in a retractable soft silicone tip which ensures nontraumatic contact with the retina.
DualBore SideFlo Cannula allows use of a side port for fluid injection, which eliminates the potential for retinal injury caused by a fluid jet stream. Multiple fluid egress vents allow fast pressure relief during injection. It is optimized for perfluorcarbon liquid and dye injections.
For scleral buckling, the El Rayes Suprachoroidal Catheter has been recently introduced for ease of use and better safety.
Steerable Laser Probe is now available by Katalyst Surgical which offers a 90˚ steerability and features a reusable handle and disposable fiber.
ILM Forceps with Eckardt tip and single movable Kamei sweeper blades have been made recently available. These are supposed to be ideal for young surgeons. Another forceps to make retinal visualization easy is the invisible forceps
Finesse Flex Loop (Alcon, Novartis, Fort Worth, US) is a curved Nitinol loop with 82 tines. The instrument’s concave shape retards penetration proportional to the amount of indentation; the design allows no more than 85% penetration into the internal limiting membrane (ILM). The loop is adjustable in order to change the stiffness. The loop has the potential to be used for IOL retrieval and hyaloid removal.
Finesse Flex Loop
3. Lenses
Single-Use Sterile Lenses: Sensor medical technology have introduced sterile disposable vitrectomy lenses for use in the office and the operating theatre. The lenses include a plano lens, a magnifier lens, a biconcave lens, a 20˚ prism lens, a 30˚ prism lens, a suture ring, and a suture ring with tabs.
Super View Disposable HTC: The Hassan-Tornambe Disposable Contact Lens is a single-use planoconcave contact lens with a 36˚ field of view. It incorporates an absorbent symmetrical foam ring with four supporting legs for increased stability during surgery.
4. 3D visualisation of vitreoretina surgery
A new concept that has garnered a great deal of attention during the past few years is 3D visualisation for vitreoretinal surgery. This is slated to provide a remarkable combination of both increased magnification and increased depth of field as compared to viewing through the optics of a microscope. While there may not be a specific ergonomic benefit, the much lower endoilluminator levels required, due to high sensitivity of the CMOS camera which can be set at an astonishingly low 1-5% for macular surgery. This decrease has been made possible in part by the recent switch to OLED screens and high sensitivity CMOS camera and OLED illumination will go a long way in reducing phototoxicity. The image displayed on a 3D goggles can provide guidance to surgery through digital indicators, may overlay perioperative pictures and investigations onto the real time field and enhance the contrast and light for better visibility of epiretinal membranes etc.
Three primary concepts are guidance, overlay and enhancement. Guidance refers to digital indicators of an instrument’s intraocular location, helping to avoid inadvertent lens or retina touch. Overlay “makes the preoperative intraoperative”,
overlaying preoperative images such as fluorescein angiography over the intraoperative retinal image. Enhancement permits reduced illumination and allows the surgeon to see otherwise invisible features such as the fine details of an epiretinal membrane. Some of these systems are already in use and being tested currently. However they will require a learning curve and a reduction in costs to become more generally acceptable.
3D Vitreoretinal surgery
5. Retinal Robotics
Preceyes (MIOS, Lausanne, Switzerland) is the ophthalmic robotics company which was the first to perform in vivo tests. Four different robotic concepts are there in eye surgery. These include, the handheld tool, instrument co-manipulation, instrument telemanipulation and magnetic control. Each varies in the degree to which the robot can filter tremors, scale motion and allow automation. With telemanipulation, the intended goal is to use robotics to enhance existing procedures currently performed, and to allow surgeons to execute manoeuvres not possible with currently available technology.